Idiopathic Guttate Hypomelanosis- All You Need To Know!
What is idiopathic guttate hypomelanosis? Is it fatal? Skin doctors warn everyone to watch out for dark moles that could indicate skin cancer, but what about those small white spots many people notice on their arms and legs?
The “reverse freckles” are caused by a benign skin condition known as Idiopathic Guttate Hypomelanosis. The specks are not a symptom of any health problem, but they can be disturbing, especially if they come in huge numbers.
Idiopathic Guttate Hypomelanosis is a common skin condition marked by many small, white spots on the shins and forearms. It first shows up in middle-aged, fair-skinned women, but it also affects dark-skinned people who have spent a long period in the sun, and both sexes acquire it more as they age.
What is Idiopathic Guttate Hypomelanosis

Idiopathic Guttate Hypomelanosis, also called symmetrical leukoplakia progressive, is a common, benign skin condition that shows up as small, irregularly shaped, well-defined, hypopigmented porcelain white macules (2 to 5 mm flat white spots), most often on the shins and forearms.
Idiopathic means that the cause is unknown, guttate means that the spots look like teardrops, and hypomelanosis means that the spots are lighter in color. There are no rough patches on the surface. Most of the time, the trunk and face are left alone. Once present, lesions do not change in size.
Idiopathic Guttate Hypomelanosis worsens with sun exposure and, to a lesser extent, with age.
Idiopathic guttate hypomelanosis is more common in people over 40, and the number of people who have it increases with age. However, young adults can also have it. Women have them more often than men do. Because the lesions seem more common in family members, there may be a genetic link.
Idiopathic Guttate Hypomelanosis primarily affects people with fair complexion; however, it can also affect people with darker skin. It is commonly found on the shins and sun-exposed portions of the forearms, but it can also appear on the face, neck & shoulders. The white spots are often smooth, reducing regular skin patterns. However, they might be slightly scaly.
While Idiopathic Guttate Hypomelanosis is harmless, it can be visually distressing for some patients. Thus therapy may be required. As Idiopathic Guttate Hypomelanosis indicates signs of sun damage, the primary treatment should consist of teaching patients about the importance of sun protection.
Patients should be encouraged to use sunscreen daily and avoid artificial tanning beds. Topical steroids, pimecrolimus, tretinoin, and dermabrasion are some treatments that may help lessen the severity of Idiopathic Guttate Hypomelanosis.
Does Idiopathic Guttate Hypomelanosis spread?
Idiopathic Guttate Hypomelanosis is most typically seen in middle-aged, light-skinned women. However, it is becoming more common in both sexes and older dark-skinned adults with a history of long-term sun exposure. Idiopathic guttate hypomelanosis is significantly more common in women, usually beginning around the age of 30.
However, age and sun exposure increases are nearly equal in older men and women. It is unknown why Idiopathic Guttate Hypomelanosis occurs earlier in young women than in young men. Fair-skinned women are the first to develop this illness; later, as age and sun exposure increase, both sexes appear to be equally affected.
The exact cause is unknown. However, it appears to be related to the sun’s effect on melanocytes. Because skin pigmentation is caused by the combination of melanocyte and keratinocyte activity, an acquired deficiency of the epidermal melanin unit causes hypopigmentation in patients with Idiopathic Guttate Hypomelanosis. In 1967, Hamada and Saito discovered a 50% drop in melanocytes.
Is Idiopathic Guttate Hypomelanosis dangerous?
Idiopathic Guttate Hypomelanosis looks unpleasant. However, it is not dangerous. Lesions, once present, do not go away.
Idiopathic guttate hypomelanosis causes
Idiopathic Guttate Hypomelanosis has no clear cause. A skin biopsy shows that the skin cells don’t have any color (melanin) (keratinocytes). The number of cells making pigment is also decreasing (melanocytes). The skin is a little bit flatter and a little bit thinner than usual.
Histology shows that the rete ridges at the dermis and epidermis junction are flattening. There is a moderate to a marked decrease in the number of melanin granules in the basal and upper layers, and fewer DOPA-positive epidermal melanocytes exist.
The cause of Idiopathic Guttate Hypomelanosis is unknown. It is an unavoidable aspect of aging, with a gradual loss of melanocytes – a process akin to hair greying. Other theories include:
- Sun damage – the lesions look like white freckles.
- Seborrheic keratosis that is not caused by the sun – degenerative scaly patches
Other suspected causes include HLA-DQ3 genetic factors, phototherapy, and autoimmune.
Idiopathic Guttate Hypomelanosis doesn’t seem to be caused by injury or a virus. The white spots do not increase your chances of developing skin cancer.
Idiopathic Guttate Hypomelanosis symptoms
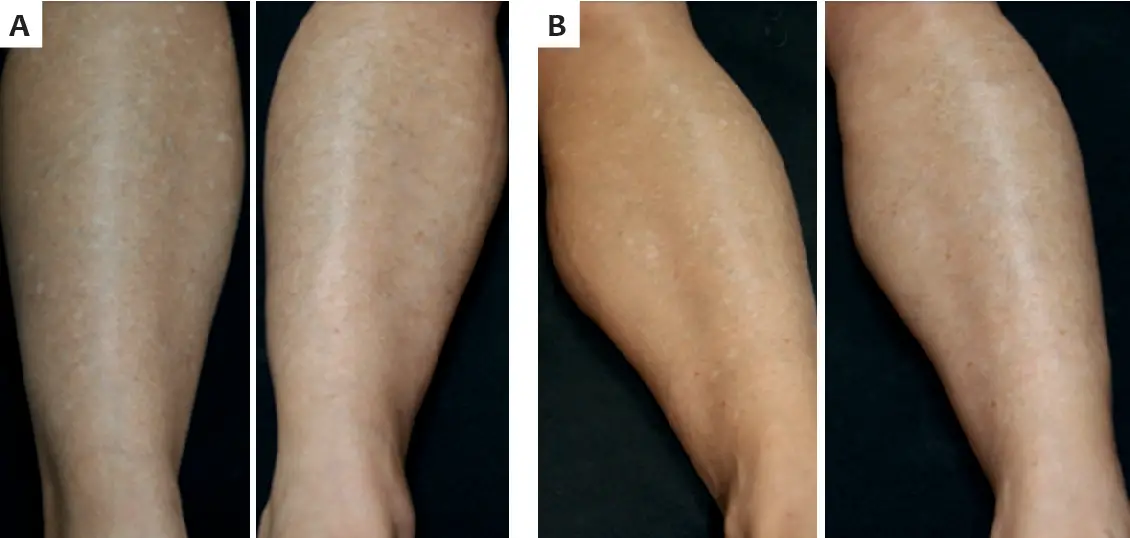
Idiopathic Guttate Hypomelanosis is a benign and symptomless skin condition that looks like white spots all over the body. The size of the lesions ranges from 1 to 10 mm, but most are between 1-3 mm.
It is particularly common in fair-skinned people and appears to be caused by repeated sun exposure rather than age. Interestingly, this illness appears earlier in women than men because their legs are more exposed. However, Idiopathic Guttate Hypomelanosis in men and women increases with age.
Idiopathic guttate hypomelanosis can be seen in elderly dark-skinned people, although usually at a later age. Most exposed parts of the body show the distribution of Idiopathic Guttate Hypomelanosis. These parts include the arms, legs, upper back, and face. Lesions are typically found along the front portion of the legs, followed by the arms, face, and back.
Idiopathic guttate hypomelanosis diagnosis
Idiopathic Guttate Hypomelanosis can only be diagnosed in the clinic by looking at the skin. Biopsies can be done, but most of the time, they are not needed. Histology shows that the rete ridges at the dermis and epidermis junction are flattening. There is a moderate to the marked decrease in the number of melanin granules in the basal and superficial layers, and there are fewer DOPA-positive epidermal melanocytes.
Idiopathic guttate hypomelanosis treatment
Most of the time, no treatment is required because the marks are harmless. Attempts to remove the lesions may leave brown or larger white markings that appear worse than the original problem. Sun protection is crucial.
The following measures may improve the appearance.
- Broad-spectrum sunscreens (SPF 50+)
- Carbon dioxide laser
- Light cryotherapy
- Chemical peel (trichloroacetic acid and phenol)
- Microdermabrasion or Localized superficial dermabrasion
- Topical tretinoin cream
- Pinch grafts of normally pigmented skin
- Topical pimecrolimus 1%
- Topical steroids
- Cosmetic cover-up
Patients should be informed that their therapy options are limited and mixed results. Sun protection can aid in the prevention of new lesions. If cryotherapy is used, patients should know the possibility of post-treatment hypopigmentation. In addition, if a patient has a history of hypertrophic scars or keloids, a test should be performed before treating all lesions with superficial dermabrasion.
Idiopathic Guttate Hypomelanosis has few treatment options. The majority of remedies are anecdotal, with no randomized controlled clinical research. A conservative approach involving monitoring and photoprotection may help avoid forming new lesions.
In one trial, tretinoin cream taken daily for four months showed some reduction in pigmentation. This study employed 0.025 percent tretinoin cream nightly for the first week, 0.05 percent nightly for the second week, and 0.1 percent nightly for the rest of the trial. In another small research, 1% pimecrolimus cream applied twice daily for 16 weeks showed some improvement in pigmentation.
Cryotherapy has been shown to help with the treatment of Idiopathic Guttate Hypomelanosis. After one study, treated lesions pigmented in 6-8 weeks and histologically had more DOPA-positive melanocytes than untreated lesions but less than normal skin.
Another small study found that therapy with local superficial dermabrasion resulted in repigmentation in 80% of treated patients. Treatments including carbon dioxide laser and superficial chemical peels have been used with limited results.
Cover-up cosmetics and concealers from brands like Dermablend can also be used to hide the hypopigmented macules.
Reducing Your Chances of Getting IGH Spots
- Wear sunscreen every day. Dermatologists still don’t know everything about what causes IGH, but they all agree that long-term sun exposure is a major factor in almost every case. Put on a broad-spectrum sunscreen every time you go outside, even on cloudy days, to protect your skin from the sun’s UV rays. IGH spots often show up in places that get a lot of UV light from the sun, like the lower legs and arms, the face, and the back of the neck.
- Cover exposed skin. Along with sunscreen, it’s a good idea to wear a wide-brimmed hat and sunglasses when you go outside to protect your head, face, and eyes. You might also want to wear long sleeves and pants on sunny days. Check the labels to find hats and clothes made of fabrics that protect against UVA and UVB rays. Don’t go outside between 10 a.m. and 4 p.m., when the sun is at its strongest.
- Don’t use tanning beds. Your current desire for a deep tan may result in a plethora of small white spots on your skin later on. Tanning beds can cause various skin problems and should be avoided at all costs. People who use tanning beds frequently before age 35 have a 75% increased chance of developing melanoma (skin cancer).
- Maintain a healthy immune system- Autoimmune problems predispose you to IGH, so do everything you can to maintain a healthy immune system. If you have an autoimmune problem, consult your doctor immediately.
- Avoid skin trauma- Skin trauma might also predispose you to IGH, protecting your skin from damage as much as possible. Get immediate medical attention if you sustain a skin injury, such as a burn or a cut.
- See if IGH runs in your family. Even if you use every advised sun protection measure, genetics may cause IGH patches. Experts aren’t sure why, but IGH appears to run in families. However, if this is the case for you, don’t use it as an excuse to skip out on sun protection. IGH spots are more common in those with fair complexion, although they are more visible in people with dark skin.
Final words:

Because Idiopathic Guttate Hypomelanosis is an autoimmune disorder, you may want to look into several autoimmune treatment options, including dietary and lifestyle changes. It would help if you also had your doctor examine for underlying disorders, including SIBO, dysbiosis, leaky gut, and systemic infections like candida.
FAQs
1. What causes Idiopathic Guttate Hypomelanosis?
Idiopathic Guttate Hypomelanosis is caused by a lack of pigmentary solar protection and sun exposure rather than age. Fair-skinned women are the first to develop this condition; later, as age and sun exposure increase, both sexes appear to be equally affected.
2. Can you treat Idiopathic Guttate Hypomelanosis?
Idiopathic guttate hypomelanosis is a common skin condition people get as they age. It is marked by many small, round, porcelain-white spots on the extensor sides of the extremities. Most people are told that the condition is harmless and no treatment is recommended.
3. How do you fix Idiopathic Guttate Hypomelanosis?
- Topical treatments — topical steroid, tacrolimus, topical retinoids.
- Cryotherapy — 5 seconds, single session, repigmentation visible by 4 months.
- Procedural treatments — chemical peel, excimer laser, skin grafting.
4. Is there treatment for IGH?
Idiopathic Guttate Hypomelanosis (IGH) is an acquired skin disease characterized by tiny hypopigmented macules on sun-exposed areas of the skin. Corticosteroids, topical or intralesional, topical retinoids, topical calcineurin inhibitors, and surgical procedures are all used to treat IGH.
5. Which vitamin deficit causes white spots on the skin?
Calcium, vitamin D, and vitamin E deficiencies can result in white patches on the skin. While these white spots are not harmful, they indicate that you should consume a healthy, balanced diet.
6. Is IGH vitiligo?
IGH is clinically often confused with vitiligo and lichen sclerosus. Histologically, both disorders have flat epidermis with considerably diminished or missing melanin in the basal layer and decreased numbers of melanocytes at the dermo-epidermal interface, identical to IGH.
7. Does Idiopathic Guttate Hypomelanosis spread?
Idiopathic Guttate Hypomelanosis typically appears in early adulthood on the legs of fair-skinned women. It may later spread to other sun-exposed areas, such as the arms and upper back.
8. Does sunscreen prevent Idiopathic Guttate Hypomelanosis?
Whatever treatment method you pick, experts agree that sunscreen is the best choice for preventing IGH and decreasing the appearance and progression of white spots on the skin.